Abu Dhabi’s primary care system is different from neighbouring Dubai’s. But it’s also different from last year’s Abu Dhabi primary care system. I learned this and more from fellow panelists and Steve Gardner in yesterday’s Healthcare World panel on primary care.
Dr. Ibtesam AlBastaki said Dubai Health Authority uses general practice in a gatekeeper model. By contrast mariam almansoori described the polyclinic model of the Department of Health Abu Dhabi. Citizens go to GPs as they make conveniently fast referrals to specialists in the same office.
Too few people took up free screening. This is expensive. 61% of Abu Dhabi’s generous budget was for curative care, only 1% for preventative care. So this year, citizens cannot get free curative care until they have attended the preventative care appointments.
Speaking to Methven Forbes before the panel, I love that people like him exist. 20 years ago, looking for a challenge, he took over a failing GP surgery looking after 4,500 people. He turned it around and today the Fuller & Forbes Healthcare Group looks after 120,000 people. NHS England pays just £163.65 per person per year. The upside for turning around a surgery is so little, the downside of failing can be so large. People like Methven deliver this in very human ways. He won’t centralise phone centre staff for example as it quickly translates to bad service – a local receptionist does so much more than booking an appointment – which becomes bad business.
Norway tries to reduce missed appointments by charging a fee. But with a €150 annual limit to protect the poor, patients do not show in 8% of appointments. That’s 500,000 people a year, said Emir Brdakic from Convene, in a country with a 400,000 person waiting list. Turkey’s private insurance model allows patients to go directly to a specialist, said Recai Serdar Gemici from Albert Health. So 6% of appointments are unnecessary as patients choose the wrong specialty.
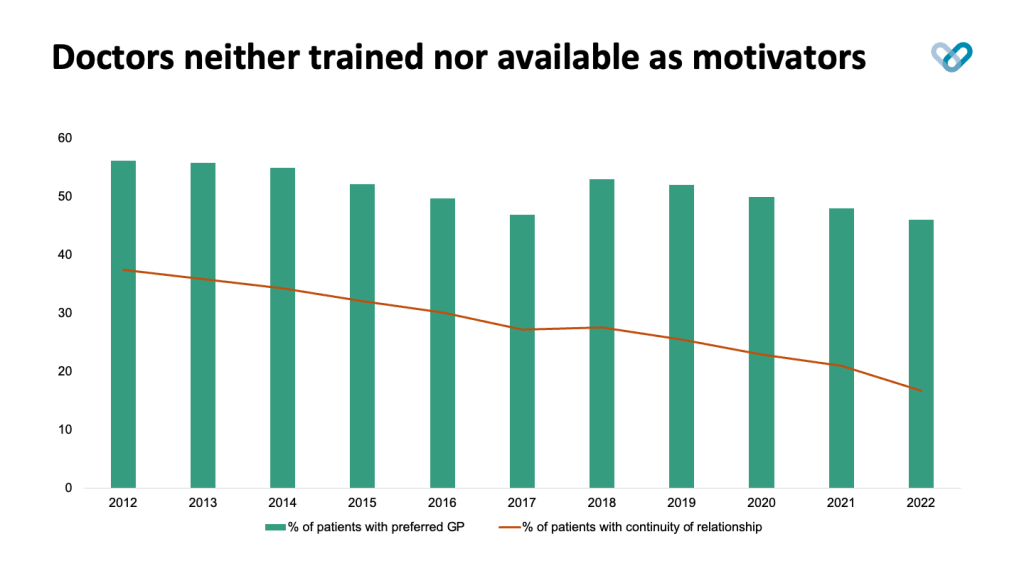
I discussed the irreversible reduction of continuity of relationships. Around 50% of patients prefer a particular GP in their surgery in England. But only 38% of patients got to see the GP they preferred in 2012, and this plummeted to 17% in 2022. We know that continuity of relationship means continuity of care and that means better clinical outcomes. We also know every other trend continues the drop in continuity of relationships.
Technology is the only path forward. That’s why later this year Patients Know Bes will show the patient the advice their GP did not have time to tell them so they can arrange the care they need. This will benefit the GP and the patient. It is critical for the future of primary care.
I am speaking today about “Empowering the Future of Wellness: Personalized Health Insights and the Shift to Preventative Care”. Join me at the World of Wellness at 3 pm at the Al Mustaqbal Hall on the last day of Arab Health Exhibition.
Discover more from CEO blog at Patients know best
Subscribe to get the latest posts sent to your email.
